Outcome of a patient with Herlyn-Werner-Wunderlich syndrome treated with Balloon septostomy – pre- and postsurgical ultrasound findings
Výsledok pacientky s Herlyn-Werner-Wunderlichovým syndrómom liečenej balónikovou septostómiou – pred - a pooperačný ultrazvukový nález
Herlyn-Werner-Wunderlichov syndróm je vzácna kongenitálna anomália, definovaná triádou vrodených chýb ženského urogenitálneho traktu – homolaterálnou renálnou agenéziou, uterom duplex a obštrukčným hemihematometrokolpom, ktorej etiológia zostáva zatiaľ nejasná. Najčastejšími klinickými príznakmi sú panvová bolesť, dysmenorrhea a hmatateľná hmota v dôsledku hematokolpu alebo hematometra. Vzhľadom na nedávne štúdie sa u týchto mladých pacientok považuje za dominantný nález endometrióza, čo môže vysvetľovať patofyziologický mechanizmus jej vzniku ako výsledok retrográdnej menštruácie. Včasná diagnostika a následná liečba sú dôležité v prevencii rozvoja závažných komplikácií. Klinické a reprodukčné výsledky po drenáži hematometrokolpu sú vo všeobecnosti uspokojivé. Predstavujeme 13-ročnú pacientku s panvovou bolesťou a diagnostikovaným syndrómom OHVIRA liečenú balónikovou septostómiou.
Authors:
Erik Dosedla 1
; Zuzana Ballová 1
; Petra Gašparová 1
; Martina Sitáš 1
; P. Calda 2
Authors‘ workplace:
Department of Gynaecology and Obstetrics, Faculty of Medicine, Pavol Jozef Safarik University in Kosice, Hospital AGEL Košice-Šaca Inc., Košice-Šaca, Slovak Republic
1; Department of Gynaecology and Obstetrics, First Faculty of Medicine, Charles University and General Teaching Hospital, Prague, Czech Republic
2
Published in:
Ceska Gynekol 2023; 88(6): 450-453
Category:
Case Report
Overview
Herlyn-Werner-Wunderlich syndrome is an unusual congenital anomaly defined by a triad of congenital defects of the female urogenital tract – homolateral renal agenesis, uterus duplex and obstructed hemi-hematometrocolpos whose etiology remains still unclear. Pelvic pain, dysmenorrhea and palpable mass due to the hematocolpos or hematometra are the most common clinical symptoms. Endometriosis is considered to be a prevalent finding in these young patients possibly explaining the pathophysiological mechanism of endometriosis as the result of retrograde menstruation. Early diagnosis and subsequent treatment are important to prevent the development of severe complications. In general, clinical and reproductive outcomes after drainage of the hematometrocolpos are reported to be satisfactory. A 13-year-old patient presented with pelvic pain and was diagnosed with OHVIRA syndrome treated with Balloon septostomy.
Keywords:
Herlyn-Werner-Wunderlich syndrome – hemi-hematocolpos – Mullerian anomaly – Wolffian anomaly – obstructive genital abnormality
Introduction
Herlyn-Werner-Wunderlich syndrome, sometimes referred to as the acronym OHVIRA (Obstructed Hemivagina and Ipsilateral Renal Anomaly) syndrome, is a rare congenital anomaly of the Mullerian (paramesonephric) and Wolffian (mesonephric) ducts. The anomaly is defined by a triad of congenital defects of female urogenital tract – homolateral renal agenesis, uterus duplex and obstructed hemi-hematometrocolpos [1,2].
This anomaly was first described as an anatomical disorder in 1922, but the designation of this syndrome is based on two articles, in the first of which Herlyn and Werner described ipsilateral kidney aplasia, uterus didelphys and Gartner duct cyst, and in the second article Wunderlich reported a rare anatomical anomaly of the absence of the right kidney and a bicornuate uterus and a unilateral blind hematocervix [3–5].
The incidence varies from 0.1–3.8% [6]. To date, etiology of Mullerian duct anomalies remains uncertain, because it is a heterogeneous complex characterized by a variety of clinical forms with the absence of genotype-phenotype correlation [7].
Generally, clinical and reproductive outcomes after drainage of the hematometrocolpos are reported to be good [2].
Case report
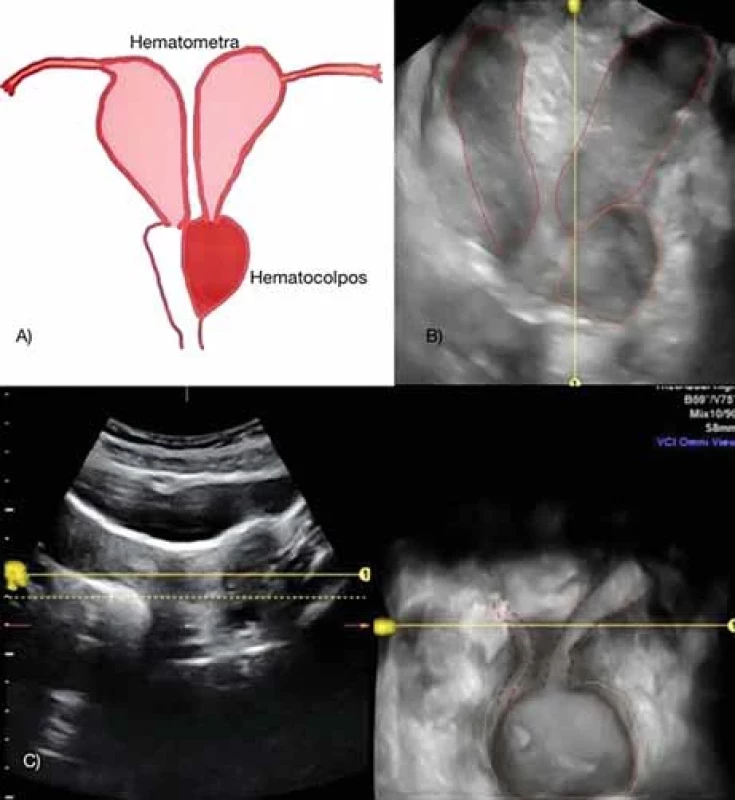
A 13-year-old female was presented to our department complaining of pelvic pain, 4-month history of dysmenorrhea and finding a hemorrhagic cyst on the left ovary. Her family history was insignificant. She was treated for epilepsy from the age of 6. Exposure to drugs, cigarettes and alcohol was negative. Her menarche was 4 months ago, with a regular but painful period. At the gynecological pelvic examination there was palpable painful resistance on the left vaginal wall. Speculum examination revealed swelling in the left vaginal vault. Upon the patient’s admission, an ultrasound examination was performed using an ultrasound system Voluson E 10 (GE Medical Systems Milwaukee, WI) equipped with a convex 4–8 MHz abdominal transducer (RAB 4–8L) and 5–9 MHz endocavity volume probe (RIC 5–9D). It revealed absence of the left kidney. Transvaginal ultrasonography revealed uterus didelphys with a single vagina and laterally, close to the left side of the vagina, a unilocular 104 × 58 mm cystic lesion with homogeneous ground glass echogenicity (Fig. 1). The cystic lesion was suspicious for hemi-hematocolpos, communicating with the left uterine cavity (dilatation 13 mm). Both ovaries were visualized and appeared normal. Due to the above mentioned ultrasound diagnosis, we assumed Herlyn-Werner--Wunderlich syndrome.
Under general anesthesia in a gynecological position, we performed a speculum examination during which the single vagina with one uterine cervix and livid bulging of the left lateral vaginal vault (hemivagina) was visualized. The right cervix was not seen, but was palpable in the sacral position on the right side of the vagina. Due to findings, we decided to create a permanent communication between the left hemi-hematocolpos and the normal vagina in order to ensure adequate drainage of the left uterus in the future. Left vaginal wall in place of the greatest bulging was grasped with Allis forceps and an opening with scissors was made (septostomy). After the incision was enlarged (Hegar dilator 5), sounding of the cervical canal and cavity of the left uterus was performed – directed obliquely to the left (ultrasound guided). The menstruation blood was aspirated by a vacuum. Using a hamornic scalpel, the opening was enlarged and the communication between the two vaginas was made. The edges of the opening were covered with a Surgicel absorbable hemostat and attached with four polyglactin 910, braided, 2-0 stitches. The 20 G Foley catheter was inserted into the left hemicolpos to maintain drainage and communication continuity.
Transvaginal ultrasound on the 1st day after surgery showed the following: the uterus was doubled, the uterus on the right was 73 × 27 mm, endometrium was 2 mm, the left uterus was 71 × 24 mm, endometrium was 1.7 mm, the right uterus connected to the right vagina, and the uterus on the left opened into the blind-ending vagina, which was atretic in the distal third of the blind-ending vagina. Inside of the left hemivagina was a balloon of the Foley catheter that properly drained the entire hematometrocolpos area (Fig. 2). The catheter was removed from the hemi-hematocolpos on the second postoperative day. The patient was discharged on the 3rd postoperative day. After surgery, she had normal regular menstrual periods.

Discussion
The pathogenesis of OHVIRA or HWW syndrome has been related to impaired development of both paramesonephric (Mullerian) and mesonephric (Wolffian) ducts [7,8].
During normal embryogenesis, by the eighth week of gestation, the Mullerian ducts migrate to the midline and fuse to form the uterus, cervix and upper vagina. The cranial end of the fused ducts forms the future uterus and cervix; the caudal end approaches the posterior wall of the urogenital sinus to form the Mullerian tubercle, which will form the upper two-thirds of the vagina. The Wolffian ducts induce the normal development of Mullerian ducts in addition to giving origin to the kidneys [9]. This explains why renal tract anomalies are associated with MDA in approximately one third of cases. Abnormal development of the Wolffian ducts leads to unilateral renal agenesis and imperforate hemivagina, which is associated with OHVIRA syndrome. On the side where the Wolffian duct is absent, the Mullerian duct is displaced laterally and cannot fuse with the contralateral duct, resulting in uterus didelphys with fully developed uterine bodies and two cervices. However, the displaced Mullerian duct that cannot come into contact with the urogenital sinus leads to an imperforate or obstructed hemivagina [10].
HWWS covers all three main types of genitourinary malformations. European Society of Human Reproduction and Embryology (ESHRE) and the European Society for Gynecological Endoscopy (ESGE) traditionally classifies the congenital anomalies of the HWWS as U3c (bicorporal uterus, bicorporal septate), C2 (double ‘‘normal’’ cervix), and V2 (longitudinal obstructing vaginal septum). However, Chinese classification of the HWWS based on morphological features of the vaginal septum, first reported by Bian et al. in a Chinese-written manuscript, classify the vaginal septum into three types:
- type I, with an imperforate vaginal septum;
- type II, with a perforate vaginal septum;
- type III, with an imperforate vaginal septum and a cervical fistula.
This classification is not widely used in English-written literature. Based on the newest study of HWWS patients from Zhu et al. in 2022, HWWS can be classified into two new types. The classification includes two main classes with subtypes.
Classification 1 contains a completely obstructed hemivagina with blind hemivagina (type 1.1) or cervicovaginal atresia without communicating uteri (type 1.2). Classification 2 comprises of an incompletely obstructed hemivagina either with partial reabsorption of the vaginal septum (type 2.1) or with communicating uteri (type 2.2) [11].
The most common clinical findings in HWWS are pelvic pain, dysmenorrhea and palpable mass due to the hematocolpos or hematometra. Pelvic pain is generally intermittent and worsens during menses. Primary amenorrhea, dyspareunia, urinary retention, spontaneous rupture of the hematocolpos, infertility, and obstetric complications are less common manifestations. Most patients present with non-specific post-pubertal symptoms, generally from 2 to 12 months after menarche. The manifestations are more painful when there is complete obstruction. If there is no complete obstruction, symptoms may be delayed or be mild. Pelvic endometriosis and pelvic infection are common complications [6,9,12]. Tong et al. reported that 18 out of 94 patients with HWWS in their study were diagnosed with pelvic endometriosis. The occurrence of pelvic endometriosis was significantly higher in patients that had HWWS with complete hemivaginal obstruction than in those with incomplete obstructions [6]. In the case of HWWS, the pathophysiological mechanism of endometriosis is retrograde menstruation [11]. Moreover, out of these 18 patients, 14 had ovarian endometrial cysts ipsilateral to the vaginal septum and 4 had bilateral ovarian endometrial cysts. The principal findings of their study are that pelvic endometriosis in adolescents should be highly suspected with an obstructive genital abnormality, and thus there could exist a close relationship between pelvic endometriosis and HWWS. Therefore, early diagnosis and subsequent treatment is very important to prevent the development of severe endometriosis in young women [6,12].
Conclusion
Like our case, patients with pelvic pain, dysmenorrhea and palpable mass are sent to the hospital for surgical treatment of an apparent hemorrhagic ovarian cyst; however, in the case of a preoperative misdiagnosis, the improper surgical procedure can cause significant bleeding from the uterus, while such cases often end in a hysterectomy, and this damages the reproductive health of the woman. Sometimes thinking out of the box is appropriate. It is recommended to implement procedures and treatment strategies from different specialties.
ORCID authors
E. Dosedla 0000-0001-8319-9008
Z. Ballová 0000-0002-0605-948X
P. Gašparová 0000-0002-6354-6911
M. Sitáš 0000-0002-7273-1051
P. Calda 0000-0002-2903-5026
Submitted/Doručené: 20. 6. 2023
Accepted/Prijaté: 17. 8. 2023
Assoc. Prof. Erik Dosedla, MD, PhD
Department of Gynaecology and Obstetrics
Faculty of Medicine
Pavol Jozef Safarik University
Hospital AGEL Košice-Šaca Inc.
Lúčna 57
040 15 Košice-Šaca
Slovak Republic
erik.dosedla@nke.agel.sk
Sources
1. Fachin CG, Rocha JL, Maltoni AA et al. Herlyn--Werner-Wunderlich syndrome: diagnosis and treatment of an atypical case and review of literature. Int J Surg Case Rep 2019; 63 : 129–134. doi: 10.1016/j.ijscr.2019.08.035.
2. Ugurlucan FG, Bastu E, Gulsen G et al. OHVIRA syndrome presenting with acute abdomen: a case report and review of the literature. Clin Imaging 2014; 38 (3): 357–359. doi: 10.1016/j.clinimag.2013.12.011.
3. Purslow CE. A case of unilateral haematocolps, haematometria, and haematosalpinx. J Obstet Gynaecol Br Emp 1922; 29 : 643. doi: 10.1111/j.1471-0528.1922.tb16100.x.
4. Herlyn U, Werner H. Simultaneous occurrence of an open Gartner-duct cyst, a homolateral aplasia of the kidney and a double uterus as a typical syndrome of abnormalities. Geburtshilfe Frauenheilkd 1971; 31 (4): 340–347.
5. Wunderlich M. Unusual form of genital malformation with aplasia of the right kidney. Zentralbl Gynakol 1976; 98 (9): 559–562.
6. Tong J, Zhu L, Chen N et al. Endometriosis in association with Herlyn-Werner-Wunderlich syndrome. Fertil Steril 2014; 102 (3): 790–794. doi: 10.1016/j.fertnstert.2014.05.025.
7. González LS, Artibani M, Ahmed AA. Study ing Müllerian duct anomalies – from cataloguing phenotypes to discovering causation. Dis Model Mech 2021; 14 (6): dmm047977. doi: 10.1242/dmm.047977.
8. Duncan PA, Shapiro LR, Stangel JJ et al. The MURCS association: Müllerian duct aplasia, renal aplasia, and cervicothoracic somite dysplasia. J Pediatr 2020; 95 (3): 399–402. doi: 10.1016/s0022-3476 (79) 80514-4.
9. Dias JL, Jogo R. Herlyn-Werner-Wunderlich syndrome: pre - and post-surgical MRI and US findings. Abdom Imaging 2015; 40 (7): 2667–2682. doi: 10.1007/s00261-015-0421-0.
10. Cunha GR, Robboy SJ, Kurita T et al. Development of the human female reproductive tract. Differentiation 2018; 103 : 46–65. doi: 10.1016/ j.diff.2018.09.001.
11. Zhu L, Chen N, Tong JL et al. New classification of Herlyn-Werner-Wunderlich syndrome. Chin Med J (Engl) 2015; 128 (2): 222–225. doi: 10.4103/0366-6999.149208.
12. Sourial S, Tempest N, Hapangama DK. Theories on the pathogenesis of endometriosis. Int J Reprod Med 2014; 2014 : 179515. doi: 10.1155/ 2014/179515.
Labels
Paediatric gynaecology Gynaecology and obstetrics Reproduction medicineArticle was published in
Czech Gynaecology

2023 Issue 6
-
All articles in this issue
- Is there a difference between acute appendicitis in pregnant and non-pregnant women?
- Are the serum delta neutrophil index and systemic inflammatory index useful as predictive parameters for preeclampsia and HELLP syndrome?
- Medical Termination of Pregnancy (MToP) in the 1st trimester – the role of human chorionic gonadotropin and ultrasound in pregnancy diagnosis and MToP follow-up
- Pregnancy termination indications and outcomes before 24 weeks of gestation – a case series
- An updated perspective on diagnostics and treatment of idiopathic granulomatous mastitis
- A rare case of a live abdominal pregnancy in a woman with subsequent gestation in utero
- DNA analysis of partial hydatidiform mole revealing triandric monogynic tetraploidy
- Outcome of a patient with Herlyn-Werner-Wunderlich syndrome treated with Balloon septostomy – pre- and postsurgical ultrasound findings
- Methods and techniques of fertility preservation in patients with endometriosis
- Assisted oocyte activation
- Effect of pelvic floor status on the outcome of pelvic organ prolapse surgery
- Preeclampsia and diabetes mellitus
- Diagnosis of complicated gynaecological inflammations by computed tomography – one center experience
- Emergent hysterectomy for placenta accreta spectrum – some additional techniques
- Diagnostika a léčba endometriózy: Doporučený postup Sekce pro léčbu endometriózy ČGPS ČLS JEP
- Czech Gynaecology
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Diagnostika a léčba endometriózy: Doporučený postup Sekce pro léčbu endometriózy ČGPS ČLS JEP
- Preeclampsia and diabetes mellitus
- Assisted oocyte activation
- Is there a difference between acute appendicitis in pregnant and non-pregnant women?
